What happens during the dying process? This question, while universally relevant, often remains shrouded in mystery and apprehension. Understanding the physical, emotional, and spiritual transitions involved can bring comfort and clarity, both for those nearing the end of life and their loved ones. This exploration delves into the multifaceted nature of death, examining the physiological changes, cognitive shifts, spiritual considerations, and the vital role of family support throughout this deeply personal journey.
From the gradual slowing of bodily functions to the complex emotional landscape experienced by both the dying individual and their family, the dying process is a unique and profoundly human experience. We will consider various perspectives on end-of-life care, address common anxieties surrounding death, and highlight the importance of compassionate communication and support during this challenging time.
Spiritual and Existential Concerns During the Dying Process
Facing mortality often prompts profound spiritual and existential reflection. The approach of death can trigger a reevaluation of one’s life, beliefs, and place in the universe, leading to a range of emotional and spiritual experiences. These experiences are deeply personal and vary significantly based on individual backgrounds, beliefs, and cultural contexts.
Spiritual and Existential Questions at the End of Life
Individuals nearing death frequently grapple with fundamental questions about the meaning of life, the nature of existence, and what, if anything, lies beyond. These questions can range from the intensely personal – “Did I live a meaningful life?” – to broader inquiries about the purpose of suffering and the universe’s ultimate design. The intensity of these questions can be heightened by the physical limitations and anxieties associated with the dying process itself.
For some, the contemplation of death brings a sense of peace and acceptance; for others, it triggers profound fear and uncertainty.
The Role of Faith and Belief Systems
For many, faith and established belief systems provide a crucial source of comfort and meaning during this challenging time. Religious or spiritual practices, such as prayer, meditation, or ritualistic observances, can offer solace, hope, and a framework for understanding death and the afterlife. The belief in a higher power, reincarnation, or an eternal soul can alleviate anxieties about death’s finality and provide a sense of continuity beyond the physical realm.
Examples include individuals finding comfort in reciting religious scriptures, engaging in spiritual practices like chanting, or receiving pastoral care from religious leaders. The specific practices and beliefs vary considerably across different faiths and spiritual traditions.
Common Fears and Anxieties Related to Death and the Afterlife
The fear of death is a universal human experience, but the specific anxieties vary greatly. Common fears include the pain and suffering associated with dying, the unknown nature of what happens after death, and the impact of one’s death on loved ones. The fear of non-existence, of ceasing to be, is a particularly profound anxiety for some. Others may fear a judgment or punishment in an afterlife.
These fears can be exacerbated by physical discomfort, cognitive decline, or social isolation. Addressing these anxieties often requires compassionate communication, emotional support, and a willingness to engage in open and honest conversations about death and dying.
Cultural Perspectives on Death and Dying
Cultural beliefs and practices profoundly shape how individuals approach death and dying. In some cultures, death is viewed as a transition to another realm, often involving elaborate rituals and ceremonies designed to guide the deceased’s spirit. For example, in many Asian cultures, ancestor veneration plays a significant role, emphasizing the continuity of family and lineage across generations. In contrast, other cultures may emphasize the importance of celebrating the life of the deceased, focusing on memories and shared experiences.
Western cultures, while diverse, often involve more individualistic approaches to death, with a focus on personal legacies and the impact on immediate family. These differing perspectives highlight the wide spectrum of human responses to mortality and the importance of cultural sensitivity in end-of-life care.
The Role of Family and Loved Ones During the Dying Process: What Happens During The Dying Process
The dying process profoundly impacts not only the individual nearing the end of life but also their family and loved ones. Navigating this challenging time requires understanding the emotional and practical burdens faced by caregivers and developing effective strategies for support and communication. Providing a comfortable and supportive environment is paramount, and careful planning for end-of-life care, including the exploration of palliative care options, can significantly ease the transition.
Family members and caregivers often experience a complex array of emotions during the dying process. Grief, anxiety, and fear are common, often intertwining with feelings of guilt, helplessness, and even anger. Practical challenges include managing the physical needs of the dying person, coordinating medical care, and making difficult decisions regarding treatment and end-of-life care. Financial burdens and the disruption of daily routines can add further stress.
The emotional toll can be significant, leading to exhaustion and impacting the mental and physical well-being of caregivers.
Effective Communication Strategies for Supporting the Dying Person and Each Other, What happens during the dying process
Open and honest communication is crucial during this period. Family members should strive to create a safe space where the dying person can express their feelings, fears, and wishes without judgment. Active listening, empathetic responses, and validation of their emotions are essential. For caregivers, open communication among themselves is equally important, allowing for the sharing of burdens, concerns, and support.
Regular family meetings can facilitate this process, providing a structured environment for discussion and decision-making. Seeking professional support from grief counselors or support groups can also provide invaluable assistance in navigating these complex emotional landscapes.
Creating a Comfortable and Supportive Environment
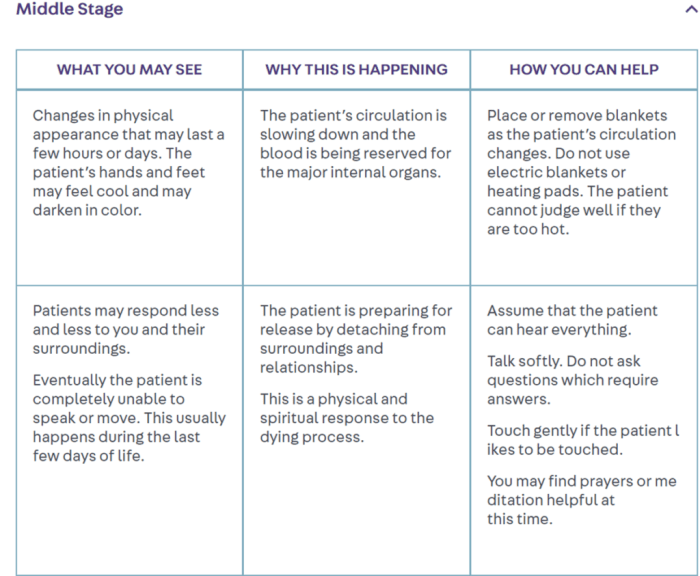
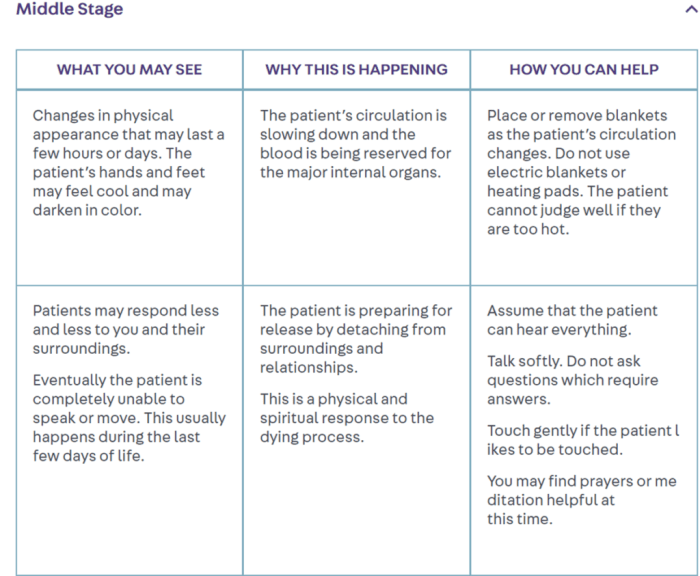
Providing a comfortable and supportive environment focuses on both physical and emotional well-being. Physically, this may involve ensuring pain management, providing assistance with personal care, and creating a peaceful and relaxing atmosphere. This could include adjusting room temperature, playing calming music, or using aromatherapy. Emotionally, it means offering unconditional love, acceptance, and companionship. Spending quality time, reminiscing about shared memories, and simply being present can provide comfort and reassurance.
Respecting the dying person’s wishes and autonomy is paramount. This includes respecting their choices regarding medical treatment, visitors, and end-of-life rituals.
Planning for End-of-Life Care, Including Palliative Care Options
Proactive planning for end-of-life care can significantly reduce stress and anxiety for both the dying person and their family. This involves addressing legal and financial matters, such as advance directives (living wills and durable power of attorney for healthcare) and making arrangements for funeral or memorial services. Exploring palliative care options is crucial. Palliative care focuses on improving the quality of life for individuals with serious illnesses, addressing their physical, emotional, and spiritual needs.
Palliative care teams can provide pain management, symptom relief, emotional support, and spiritual guidance, working collaboratively with the family and other healthcare providers to create a holistic and compassionate care plan. Early engagement with palliative care services can allow for better planning and preparation, minimizing distress and ensuring the dying person’s comfort and dignity are prioritized.
Death and Dying

Death and dying are universal human experiences, yet each individual’s journey is unique. Understanding the broader context surrounding this process, including the stages of grief, end-of-life care options, and ethical considerations, can provide valuable support and guidance for both those facing death and their loved ones.
Stages of Grief and Bereavement
The grieving process is not linear; individuals may experience these stages in different orders, intensities, and durations. Elisabeth Kübler-Ross’s five stages – denial, anger, bargaining, depression, and acceptance – offer a framework, but it’s crucial to remember that not everyone experiences all stages, and the order is not fixed. Grief is a deeply personal journey, influenced by individual personalities, cultural backgrounds, and the nature of the loss.
Support systems play a crucial role in navigating this complex emotional landscape.
Approaches to End-of-Life Care
Hospice care and hospital care represent contrasting approaches to end-of-life management. Hospice focuses on providing comfort and support to individuals with terminal illnesses and their families, emphasizing quality of life over curative treatment. It typically takes place at home, in a hospice facility, or in a nursing home. In contrast, hospital care often prioritizes aggressive medical interventions aimed at prolonging life, even if it means increased discomfort or reduced quality of life.
The choice between these approaches depends on individual preferences, prognosis, and available resources. Many individuals opt for a combination of approaches, utilizing hospital care for acute needs and transitioning to hospice for palliative care.
Ethical Considerations Surrounding End-of-Life Decisions
Advance directives, such as living wills and durable powers of attorney for healthcare, allow individuals to express their wishes regarding medical treatment in the event they become incapacitated. These documents play a crucial role in ensuring patient autonomy and preventing unwanted medical interventions. Assisted dying, a highly debated topic, involves providing medical assistance to end one’s life under specific circumstances.
The legality and ethical implications of assisted dying vary widely across jurisdictions, sparking ongoing discussions about individual rights, physician responsibility, and the definition of a “good death.” These decisions are deeply personal and should be made with careful consideration of ethical, legal, and personal values.
“The moment of death is not an ending, but a transformation. It’s a shedding of the physical form, a release into the boundless unknown. While grief is a natural response to loss, the love shared remains, woven into the fabric of memory, forever altering our perspective and enriching our lives.”
Ultimately, understanding what happens during the dying process offers a valuable opportunity for preparation, acceptance, and meaningful connection. By acknowledging the physical, emotional, and spiritual aspects of this final transition, we can foster a more compassionate and supportive environment for both the dying person and their loved ones. Open communication, access to appropriate care, and a focus on honoring the individual’s wishes are paramount in ensuring a peaceful and dignified end-of-life experience.
The journey, while deeply personal, can be navigated with greater understanding and empathy through informed preparation and compassionate support.
Questions and Answers
What is the average length of the dying process?
The duration varies greatly depending on the underlying cause of death and individual factors. It can range from a few hours to several weeks or months.
Can a dying person still hear me?
Yes, even if they appear unresponsive, it’s believed that hearing is often one of the last senses to go. Continue speaking to them, sharing memories, and offering comfort.
What are the signs of approaching death?
These can include decreased alertness, changes in breathing patterns (Cheyne-Stokes respiration), changes in skin color and temperature, and decreased urine output. These are not always present in every case.
How can I help a loved one who is dying?
Provide comfort, listen to their concerns, offer physical support as needed, and be present. Seek support for yourself as well.






