
Understanding euthanasia and assisted death requires navigating complex ethical, legal, and medical landscapes. This exploration delves into the nuanced definitions of these end-of-life practices, examining the critical distinctions between voluntary, involuntary, and non-voluntary euthanasia, as well as the legal variations across jurisdictions. We will also consider the crucial role of palliative care in managing suffering, the medical criteria for eligibility, and the procedures involved.
Furthermore, we will weigh the ethical and religious perspectives, acknowledging the diverse viewpoints and the central concept of patient autonomy.
The discussion will also encompass the broader societal implications of legalizing euthanasia and assisted dying, including potential impacts on vulnerable populations and the influence of public opinion. Finally, we will examine the stages of grief and dying, emphasizing the importance of advance care planning and the resources available to individuals and families facing these difficult decisions. This comprehensive analysis aims to provide a balanced and informative understanding of this multifaceted issue.
Defining Euthanasia and Assisted Dying

Euthanasia and physician-assisted suicide are complex and often emotionally charged topics, sparking intense debate across legal, ethical, and societal landscapes. Understanding the precise definitions of these terms is crucial for navigating this discussion responsibly. This section will clarify these definitions, highlight legal distinctions, and explore the ethical considerations surrounding them.
Defining Euthanasia, Understanding euthanasia and assisted death
Euthanasia, derived from Greek meaning “good death,” refers to the act of intentionally ending a life to relieve suffering. It’s categorized into three types based on the patient’s involvement: Voluntary euthanasia occurs when the patient explicitly requests their death; involuntary euthanasia happens when the patient is capable of expressing their wishes but their death is induced without consent; and non-voluntary euthanasia occurs when the patient is unable to express their wishes, rendering consent impossible.
The key differentiator lies in the patient’s agency and their capacity to make an informed decision.
Legal Distinctions Between Euthanasia and Physician-Assisted Suicide
While both involve ending a life to alleviate suffering, euthanasia and physician-assisted suicide differ significantly in the level of physician involvement. In euthanasia, the physician directly administers a lethal substance, actively causing the patient’s death. Physician-assisted suicide (PAS), also known as assisted dying, involves the physician providing the means for the patient to end their own life, such as a prescription for lethal medication, but the patient administers the medication themselves.
This distinction is crucial legally, as many jurisdictions that prohibit euthanasia may permit PAS under specific circumstances.
Ethical Considerations Surrounding Definitions
The ethical considerations surrounding these practices are multifaceted. Arguments for euthanasia and PAS often center on autonomy—the patient’s right to self-determination and control over their own life and death, particularly in the face of unbearable suffering. Conversely, opponents raise concerns about the sanctity of life, potential for abuse (particularly regarding vulnerable populations), and the role of physicians in preserving life rather than ending it.
The slippery slope argument, suggesting legalization could lead to unintended consequences, also features prominently in ethical debates. The definition itself is contested: what constitutes “unbearable suffering”? Who determines eligibility? These questions highlight the ethical complexities inherent in these practices.
Comparative Legal Status of Euthanasia and Assisted Suicide
The legal status of euthanasia and assisted suicide varies significantly across jurisdictions. The following table offers a snapshot, acknowledging that laws are constantly evolving and specific criteria can be nuanced:
| Jurisdiction | Legal Status of Euthanasia | Legal Status of Assisted Suicide | Key Legal Criteria |
|---|---|---|---|
| Netherlands | Legal under strict conditions | Legal under strict conditions | Terminal illness, unbearable suffering, informed consent, multiple medical consultations |
| Belgium | Legal under strict conditions | Legal under strict conditions (often considered a form of euthanasia) | Similar to Netherlands, with emphasis on unbearable and incurable suffering |
| Canada | Illegal | Legal under strict conditions | Grievous and irremediable medical condition causing intolerable suffering, informed consent, multiple medical evaluations |
| United States | Illegal (nationally) | Legal in some states (e.g., California, Oregon, Vermont) under strict conditions | Varying criteria across states, generally requiring terminal illness, unbearable suffering, informed consent, and multiple physician evaluations |
Medical Aspects of End-of-Life Care
End-of-life care encompasses a multifaceted approach to managing the physical, emotional, and spiritual needs of individuals facing terminal illness. A crucial component is the effective management of pain and suffering, often achieved through palliative care, while navigating the complex legal and ethical considerations surrounding euthanasia and assisted dying. Understanding the medical aspects of these processes is vital for informed decision-making.
Palliative Care’s Role in Managing Pain and Suffering
Palliative care focuses on providing relief from the symptoms and stress of a serious illness. It aims to improve the quality of life for both the patient and their family. This holistic approach addresses not only physical pain through medication and other interventions, but also emotional, social, and spiritual well-being. Pain management is a key aspect, utilizing a variety of methods including analgesics, non-pharmacological techniques like massage and music therapy, and psychological support to address the emotional toll of illness.
Palliative care teams work collaboratively with patients and families to develop individualized care plans, ensuring comfort and dignity throughout the end-of-life journey. For instance, a patient experiencing severe pain from advanced cancer might receive a combination of opioid medications, physiotherapy to manage mobility issues, and counseling to cope with the emotional distress.
Medical Criteria for Euthanasia or Assisted Dying Eligibility
Eligibility for euthanasia or assisted dying is typically determined based on stringent medical criteria. These criteria vary across jurisdictions but generally include a terminal illness with a prognosis of unbearable suffering and a limited life expectancy. The patient must possess decision-making capacity, meaning they understand their condition and the implications of their choice. A thorough assessment by a physician is crucial to confirm the diagnosis, prognosis, and the patient’s capacity to make an informed decision.
Additionally, some jurisdictions require a second medical opinion to ensure the appropriateness of the request. For example, a patient with amyotrophic lateral sclerosis (ALS) experiencing progressive paralysis and severe respiratory distress might meet the criteria, while someone suffering from depression, even severe depression, typically would not.
Procedures Involved in Euthanasia and Assisted Dying
Euthanasia involves a physician directly administering a lethal medication to end a patient’s life, while assisted dying involves the physician providing the means for the patient to self-administer the lethal medication. Both processes necessitate strict adherence to legal and ethical guidelines. In euthanasia, the physician carefully assesses the patient’s condition and administers the medication under controlled circumstances, ensuring a peaceful and painless death.
In assisted dying, the physician provides the medication, ensuring the patient understands the implications and has the ability to self-administer it. In both cases, thorough documentation of the process is essential.
Decision-Making Process for Patients Considering Euthanasia or Assisted Suicide
The decision to pursue euthanasia or assisted dying is deeply personal and should be made with careful consideration and support.
Ethical and Religious Perspectives
The ethical and religious considerations surrounding euthanasia and assisted dying are complex and deeply interwoven with personal beliefs, societal values, and philosophical frameworks. These practices raise fundamental questions about the value of human life, individual autonomy, and the role of medical professionals in end-of-life care. Understanding these diverse perspectives is crucial for navigating the ongoing debate and formulating informed policies.
Ethical Arguments For and Against Euthanasia and Assisted Dying
The ethical debate surrounding euthanasia and assisted dying centers on the balance between individual autonomy and the sanctity of life. Utilitarian ethics, for instance, might support these practices if they maximize overall happiness by relieving suffering, while deontological ethics, emphasizing moral duties, might oppose them due to the inherent wrongness of intentionally ending a life. Natural law theory, which posits that human actions should align with natural inclinations, generally opposes euthanasia.
| Arguments For | Arguments Against |
|---|---|
|
Religious Viewpoints on Euthanasia and Assisted Dying
Religious perspectives on euthanasia and assisted dying vary significantly. Some religions, such as certain branches of Christianity, strictly prohibit euthanasia, viewing it as a violation of God’s will and the sanctity of life. Other religions, or denominations within a religion, may adopt a more nuanced approach, acknowledging the importance of relieving suffering while emphasizing the importance of preserving life.
For example, some interpretations of Buddhism focus on compassion and minimizing suffering, which might lead to a more accepting view of euthanasia under certain circumstances. Judaism also holds a wide range of opinions, with some emphasizing the sanctity of life and others prioritizing the alleviation of suffering.
Autonomy and End-of-Life Decision-Making
The concept of autonomy, or self-governance, is central to the debate surrounding euthanasia and assisted dying. It emphasizes the individual’s right to make informed decisions about their own body and life, including the timing and manner of their death. However, the application of autonomy in end-of-life decision-making is often complicated by factors such as the patient’s capacity to make informed choices, the potential influence of family members, and the availability of adequate palliative care.
A balance must be struck between respecting individual autonomy and ensuring that decisions are made in a thoughtful and responsible manner, considering the potential consequences for the individual and society. This often necessitates careful consideration of the patient’s wishes, their mental capacity, and the availability of alternative options like palliative care.
Legal and Societal Implications
The legalization of euthanasia and assisted dying triggers complex legal and societal ramifications, impacting various aspects of life, from individual rights to the overall structure of healthcare systems. Navigating these implications requires a careful consideration of diverse perspectives and potential consequences. This section will explore the legal frameworks in different countries, analyze societal impacts, and examine the role of public opinion in shaping policy.
Legal Frameworks Governing Euthanasia and Assisted Dying
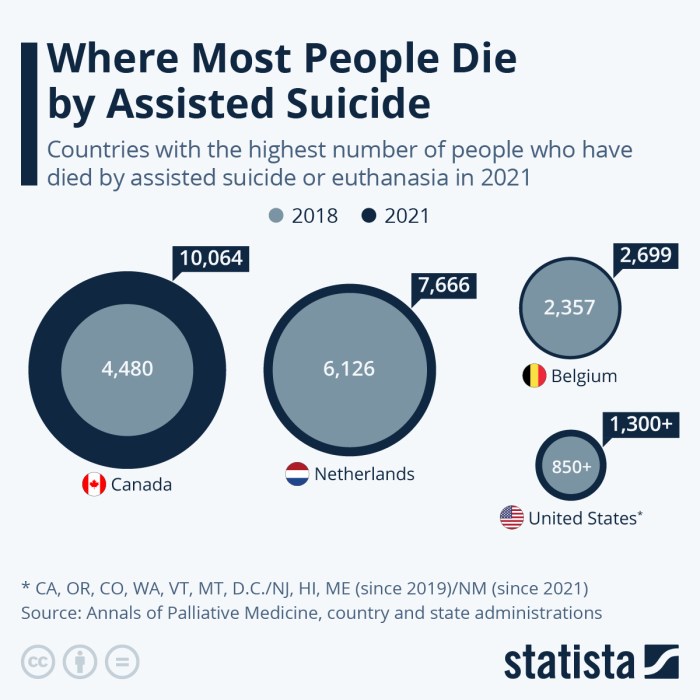
Legal frameworks governing euthanasia and assisted dying vary significantly across the globe. Some countries, such as the Netherlands, Belgium, and Canada, have legalized assisted dying under specific conditions, including terminal illness, unbearable suffering, and informed consent. These laws often include rigorous safeguards, such as multiple medical evaluations and psychological assessments, to prevent abuse. Other countries, like Germany, have more restrictive laws, permitting only the withdrawal or withholding of life-sustaining treatment.
Still others maintain outright prohibitions against euthanasia and assisted dying, often based on religious or ethical objections. These differing legal approaches reflect diverse societal values and beliefs regarding the end of life.
Societal Impacts of Legalizing Euthanasia and Assisted Dying
Legalizing euthanasia and assisted dying can have profound societal impacts. Concerns exist regarding the potential for coercion of vulnerable populations, such as the elderly or disabled individuals, who might feel pressured to choose death rather than burden their families or society. Conversely, proponents argue that legalization provides autonomy and dignity to individuals facing intractable suffering, allowing them to make choices aligned with their values.
The impact on healthcare professionals also needs careful consideration. Conscientious objection clauses are often included in legislation to protect healthcare providers who, due to religious or ethical beliefs, cannot participate in assisted dying procedures. The potential impact on insurance costs and resource allocation within healthcare systems is another area of ongoing debate.
The Role of Public Opinion and Advocacy Groups
Public opinion and advocacy groups play a crucial role in shaping policy debates surrounding end-of-life choices. Polls show varying levels of public support for euthanasia and assisted dying, often influenced by cultural and religious factors. Advocacy groups, both those supporting and opposing legalization, actively participate in public discourse, lobbying governments, and engaging in educational campaigns. Their influence on shaping legislation and public perception is undeniable, highlighting the importance of informed and respectful dialogue on this sensitive issue.
Consequences of Different Legal Approaches: Case Studies
The Netherlands, with its relatively liberal approach, provides a case study for examining the long-term consequences of legalization. While initial concerns about abuse have not materialized on a large scale, ongoing monitoring and adjustments to the legal framework are necessary to address potential vulnerabilities. Conversely, countries with more restrictive laws often face challenges in providing adequate palliative care and support for individuals facing terminal illness, potentially leading to suffering that could be alleviated through other means.
Comparing the experiences of countries with differing legal approaches offers valuable insights into the complexities and potential consequences of various policy choices. The Belgian experience, for instance, demonstrates the need for robust safeguards and ongoing ethical review to prevent potential misuse, while the Canadian experience shows the evolving nature of legal and societal adaptations to such legislation.
Death and Dying: Understanding Euthanasia And Assisted Death
Understanding death and dying extends beyond the purely medical aspects of euthanasia and assisted dying. It encompasses the emotional, psychological, and spiritual journeys of patients, their families, and healthcare providers. A holistic perspective considers the multifaceted challenges inherent in the dying process and emphasizes the importance of compassionate care and informed decision-making.
Kübler-Ross Stages of Grief and Dying
Elisabeth Kübler-Ross’s model, while not universally applicable or experienced in a linear fashion, provides a framework for understanding the emotional responses to terminal illness and impending death. These stages – denial, anger, bargaining, depression, and acceptance – represent potential emotional responses, not a prescribed sequence. Individuals may experience these stages in different orders, skip stages entirely, or revisit them multiple times.
The model highlights the complex and often unpredictable nature of the grieving process. It’s crucial to remember that these are emotional responses, and not everyone will experience all of them, nor in the same order or intensity. Support and understanding are key during this period.
Psychological and Emotional Challenges
The dying process presents significant psychological and emotional challenges for patients, families, and healthcare professionals. Patients may grapple with fear, anxiety, depression, and a sense of loss of control. Families often experience intense grief, guilt, and uncertainty, sometimes struggling to balance their own needs with the needs of the dying person. Healthcare providers face the emotional toll of witnessing suffering and loss, requiring effective coping mechanisms and access to support systems to prevent burnout.
Open communication and access to appropriate emotional support are crucial for all involved. For example, a family might struggle with the decision to withdraw life support, leading to intense guilt or conflict even after the death.
Advance Care Planning and Advance Directives
Advance care planning is the process of reflecting on and documenting one’s wishes regarding future medical care, particularly in situations where the individual may lack the capacity to make decisions. This process involves considering one’s values, goals, and preferences regarding treatment options, including life-sustaining treatments. Advance directives are legal documents that Artikel these wishes, such as living wills (specifying treatment preferences) and durable power of attorney for healthcare (designating a surrogate decision-maker).
Creating advance directives allows individuals to maintain control over their end-of-life care and reduces the burden on loved ones when making difficult decisions. A well-executed advance care plan ensures that a person’s wishes are respected, minimizing potential conflicts and promoting a more peaceful end-of-life experience.
Resources for End-of-Life Decisions
Access to information and support is vital for individuals and families navigating end-of-life decisions. Many organizations provide valuable resources, including counseling, support groups, and educational materials.
- Hospice organizations: Provide comprehensive palliative care and support for dying individuals and their families.
- National organizations focused on end-of-life care: Offer information, resources, and advocacy related to end-of-life issues.
- Religious and spiritual organizations: Provide spiritual guidance and support during the dying process.
- Grief counseling services: Offer professional support to individuals and families coping with loss.
- Online resources: Numerous websites and online communities provide information and support for those facing end-of-life decisions.
Ultimately, understanding euthanasia and assisted death necessitates a careful consideration of the ethical, legal, and personal dimensions involved. While the debate remains complex and deeply personal, a thorough examination of the medical realities, legal frameworks, and diverse perspectives allows for a more informed and compassionate approach to end-of-life care. The resources and information presented here aim to facilitate meaningful conversations and empower individuals to make informed decisions in accordance with their values and beliefs.
Open dialogue and continued exploration are crucial to fostering a society that respects the dignity and autonomy of all individuals, particularly as they approach the end of life.
FAQ Resource
What is the difference between euthanasia and physician-assisted suicide?
Euthanasia involves a physician directly administering a lethal substance to end a patient’s life. Physician-assisted suicide involves a physician providing a patient with the means to end their own life, but the patient administers the lethal substance.
Are there any situations where involuntary euthanasia is legal?
Involuntary euthanasia, where a person is killed without their consent, is illegal everywhere. It is considered murder.
What role does family consent play in euthanasia decisions?
The role of family consent varies greatly depending on jurisdiction and the patient’s capacity to make decisions. In many places, the patient’s wishes are paramount, even if family members disagree. However, family input may be considered in cases of incapacitated patients.
What are some common misconceptions about euthanasia?
Common misconceptions include the belief that euthanasia is always a quick and painless process, that it is only for the terminally ill, or that it is a solution to all end-of-life suffering. In reality, the process can be complex, and palliative care often addresses much of the suffering.






