Final wishes and advance directives are crucial for ensuring your end-of-life care aligns with your values and preferences. This exploration delves into the legal frameworks surrounding advance directives, such as living wills and durable powers of attorney for healthcare, highlighting their importance in navigating complex end-of-life decisions. We’ll examine the emotional aspects of mortality and explore practical considerations like funeral arrangements and financial planning, offering guidance on communicating your wishes effectively to loved ones and ensuring peace of mind.
Understanding these documents empowers you to make informed choices about your medical care, avoid potential family conflicts, and ensure your final wishes are respected. This guide provides a comprehensive overview of the process, from drafting and executing legal documents to fostering open communication with family and friends about sensitive topics. We will also address the practical and emotional challenges involved in end-of-life planning, offering support and resources to help navigate this important life stage.
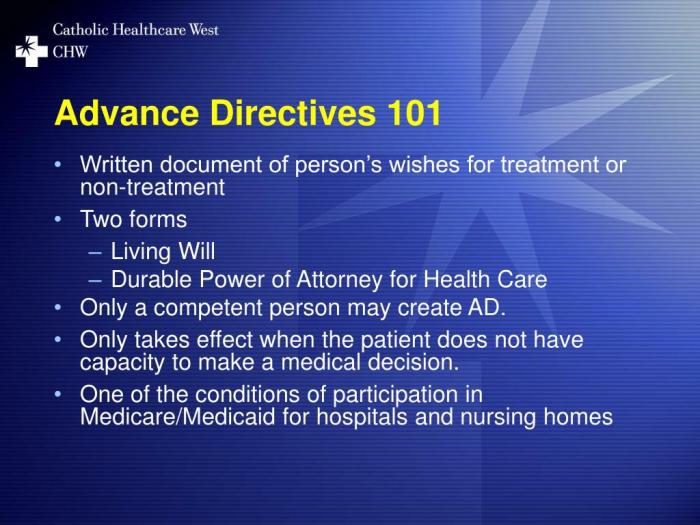
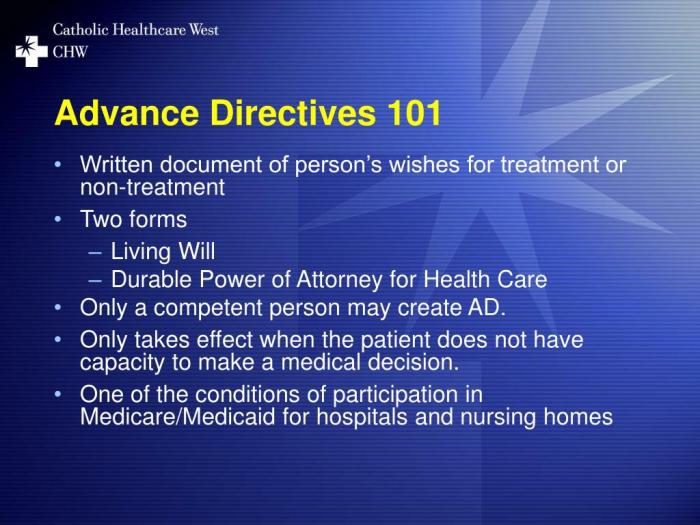
Understanding Advance Directives
Advance directives are legal documents that allow individuals to communicate their wishes regarding their healthcare and/or financial affairs should they become incapacitated and unable to make decisions for themselves. They provide a crucial mechanism for ensuring that an individual’s preferences are respected, even when they can no longer express them directly. These documents empower individuals to maintain control over their lives, even in the face of unforeseen circumstances.
Legal Definition of Advance Directives
Advance directives are defined legally as written instructions that detail an individual’s healthcare preferences or designate a surrogate decision-maker. The specific legal definition may vary slightly by state, but the core principle remains consistent: to give individuals the right to direct their future medical care and to choose who will make those decisions if they become unable to do so.
These directives are legally binding, providing guidance to healthcare providers and family members.
Types of Advance Directives
Several types of advance directives exist, each serving a distinct purpose. Common examples include living wills and durable powers of attorney for healthcare. A living will Artikels an individual’s wishes regarding medical treatment under specific circumstances, such as terminal illness or persistent vegetative state. It often addresses life-sustaining treatment, artificial nutrition and hydration, and pain management. A durable power of attorney for healthcare designates a trusted individual to make healthcare decisions on the individual’s behalf if they become incapacitated.
This agent, or healthcare proxy, has the authority to act according to the principal’s known wishes, or in the principal’s best interests if those wishes are unknown or unclear.
Creating and Executing an Advance Directive
The process of creating an advance directive generally involves consulting with an attorney or healthcare professional to ensure the document accurately reflects one’s wishes and complies with state laws. The individual completes the chosen form, clearly outlining their preferences and designating a healthcare proxy (if applicable). The document is then typically witnessed and notarized to ensure its legal validity.
Execution involves the individual signing the document in the presence of witnesses, usually two, who also sign to attest to the individual’s capacity and willingness.
Importance of Regular Review and Updates
Circumstances, values, and medical advancements change over time. Therefore, regular review and updates to advance directives are crucial to ensure they remain consistent with an individual’s current wishes. Annual review, or at least every few years, is recommended. Significant life events, such as a change in health status, marriage, or the birth of a child, may warrant more frequent review.
Failing to update an advance directive could result in medical decisions being made that are contrary to the individual’s current preferences.
Sample Durable Power of Attorney for Healthcare
The following is a sample form, and it is crucial to consult with legal counsel to create a legally sound and personalized document that complies with your state’s specific requirements.
| Principal (Person Granting Authority) | _______________________________ |
|---|---|
| Address | _______________________________ |
| Agent (Healthcare Proxy) | _______________________________ |
| Address | _______________________________ |
| Effective Date | _______________________________ |
| Grant of Authority: I, the Principal, hereby appoint the Agent to act as my attorney-in-fact for healthcare decisions. This authority shall commence upon my incapacity to make healthcare decisions and shall continue until my death or until I revoke this power of attorney in writing. | |
| Agent’s Duties: My Agent shall make healthcare decisions on my behalf in accordance with my wishes, as expressed in this document or otherwise known to my Agent. If my wishes are unknown or unclear, my Agent shall make decisions in my best interests. | |
| Specific Instructions (Optional): [Space for specific instructions regarding medical treatments, life support, etc.] | |
| Witness Signatures: | |
| Witness 1 Signature:_______________________________ | Witness 2 Signature:_______________________________ |
| Witness 1 Printed Name:_______________________________ | Witness 2 Printed Name:_______________________________ |
| Principal’s Signature:_______________________________ | |
| Date:_______________________________ | |
Final Wishes and Their Legal Implications
Planning for end-of-life care through advance directives is crucial, not only for ensuring personal wishes are respected but also to avoid potential legal complexities and family conflicts. The absence of these directives can lead to significant challenges for loved ones and create ambiguity surrounding medical treatment and asset distribution.
Legal Ramifications of Not Having Advance Directives
Without advance directives, legal decisions regarding medical treatment and the distribution of assets often fall to the courts. This process can be lengthy, expensive, and emotionally taxing for the family. The court will appoint a guardian or conservator to make decisions on behalf of the incapacitated individual, based on what the court determines to be in the person’s “best interests.” This determination may not align with the individual’s actual wishes, leading to unwanted medical interventions or an unequal distribution of assets.
Furthermore, the lack of clear instructions can result in protracted legal battles between family members contesting the decisions made on the deceased’s behalf. This often creates further emotional distress during an already difficult time.
The Role of Family Members in End-of-Life Decision-Making When Directives Are Absent
When an individual lacks advance directives, the responsibility for making end-of-life decisions typically falls to family members. However, this responsibility is not clearly defined legally and often depends on state or country-specific laws regarding hierarchy of decision-makers (e.g., spouse, adult children, parents). This can lead to significant disagreements and conflicts, particularly when family members hold differing opinions regarding the best course of action for the incapacitated individual.
The emotional strain of such decision-making, coupled with the lack of clear guidance, can further complicate an already stressful situation. In some cases, family members might be compelled to make difficult decisions under pressure, potentially leading to feelings of guilt or regret later.
Comparison of Legal Processes Across Jurisdictions Regarding Final Wishes
Legal processes concerning end-of-life decisions and the enforcement of final wishes vary significantly across different states and countries. For example, some jurisdictions prioritize the wishes of family members, while others emphasize the importance of appointed legal guardians. The availability and legal standing of specific advance directives, such as living wills or durable powers of attorney, also differ. In some countries, euthanasia or physician-assisted suicide are legal under specific circumstances, while in others they are strictly prohibited.
These variations highlight the importance of understanding the specific legal framework within one’s jurisdiction when planning for end-of-life care. Navigating these differences requires legal expertise, making it advisable to consult with an attorney specializing in estate planning and end-of-life care.
Potential Conflicts Between Family Members Regarding End-of-Life Decisions
Family conflicts regarding end-of-life decisions are common when advance directives are absent. Disagreements can arise from differing interpretations of the incapacitated individual’s wishes, personal biases, or financial motivations. Sibling rivalries, strained relationships between spouses, or conflicting beliefs about medical interventions can escalate tensions and lead to legal disputes. The emotional weight of these decisions, coupled with the potential for financial implications (e.g., inheritance disputes), often exacerbates these conflicts.
Mediation or family counseling can sometimes help resolve these disputes, but in many cases, legal intervention becomes necessary.
Comparison of Different Types of Advance Directives
| Type of Advance Directive | Description | Legal Authority | Scope |
|---|---|---|---|
| Living Will | Specifies the type of medical treatment desired or refused in the event of terminal illness or persistent vegetative state. | Varies by jurisdiction; generally requires clear and convincing evidence of intent. | Medical treatment only. |
| Durable Power of Attorney for Healthcare | Appoints a designated individual to make healthcare decisions on one’s behalf if they become incapacitated. | Varies by jurisdiction; typically requires clear and unambiguous language. | All aspects of healthcare decision-making. |
| Do Not Resuscitate (DNR) Order | Instructs medical professionals not to perform cardiopulmonary resuscitation (CPR) in the event of cardiac or respiratory arrest. | Requires physician’s signature and usually patient consent or that of their legal representative. | CPR only. |
| Last Will and Testament | Specifies how assets and property will be distributed after death. | Requires proper execution according to state laws (e.g., witnessing, notarization). | Distribution of assets and property. |
Communicating Final Wishes to Loved Ones: Final Wishes And Advance Directives

Sharing your end-of-life wishes with loved ones is a crucial step in ensuring your preferences are respected. Open communication, while challenging, fosters peace of mind for both you and your family, minimizing potential conflict and confusion during a difficult time. This process requires sensitivity, planning, and clear articulation of your desires.Effective communication strategies are essential for navigating this sensitive subject.
Approaching the conversation with empathy and understanding is paramount. It’s important to remember that your loved ones may have their own emotional responses to process, so patience and reassurance are vital.
Step-by-Step Guide to Communicating Final Wishes
Openly discussing death and dying can be uncomfortable, but a structured approach can ease the process. Begin by choosing a private and comfortable setting where you and your loved one(s) can talk openly without interruptions. Consider offering refreshments to create a more relaxed atmosphere.
- Initiate the Conversation: Start by expressing your desire to share your end-of-life wishes. You might say something like, “I’ve been thinking a lot about the future, and I want to make sure my wishes are clear.”
- Explain Your Wishes Clearly: State your preferences regarding medical treatment, funeral arrangements, and the distribution of your assets. Use simple, straightforward language, avoiding jargon. For example, “I’ve prepared advance directives outlining my wishes regarding life support,” or “I’d prefer a simple cremation with a small gathering of close family and friends.”
- Address Potential Questions and Concerns: Anticipate questions and concerns your loved ones may have and be prepared to answer them honestly and patiently. Allow them to express their feelings without judgment.
- Provide Written Documentation: Offer copies of your advance directives, will, and any other relevant documents. This provides a tangible record of your wishes, reducing ambiguity and potential disputes.
- Schedule Follow-up Conversations: Plan to revisit the topic periodically, especially after significant life changes or if your wishes evolve. This ensures your loved ones remain informed and your wishes are current.
Examples of Conversations about End-of-Life Wishes
Example 1: “Mom, Dad, I’ve created an advance directive specifying my wishes regarding medical intervention if I become terminally ill. I’d like you to read through it, and we can discuss any questions you may have.”Example 2: “John, I’ve chosen to be cremated rather than buried, and I’ve already made arrangements for a simple memorial service. I wanted to let you know so you’re aware of my preferences.”Example 3: “Sarah, I’ve updated my will to ensure my assets are distributed according to my wishes.
I’ve left a copy with my lawyer, and I’d be happy to go over the key points with you.”
The Importance of Open and Honest Communication
Open and honest communication is paramount. It prevents misunderstandings, reduces family conflict, and ensures your wishes are respected. It also allows your loved ones to process their emotions and prepare for your eventual passing, creating a more peaceful experience for everyone involved. Transparency fosters trust and strengthens family bonds, even during a challenging time.
Using Visual Aids to Aid Communication
A simple flowchart depicting the decision-making process in case of incapacitation can be helpful. For instance, a flowchart could visually represent the order of individuals who would make medical decisions on your behalf. Another visual aid could be a simple chart outlining your funeral preferences: cremation vs. burial, type of service, preferred location, etc. A color-coded chart illustrating the distribution of assets in your will could also clarify your intentions.
These visuals provide a clear, concise summary of complex information, facilitating understanding and reducing anxiety.
Death, Dying, and the Emotional Aspects
Confronting one’s own mortality is a deeply personal and complex journey, often marked by a wide range of psychological and emotional responses. Understanding these stages and the support systems available can significantly aid individuals and their families in navigating this challenging period. The process is rarely linear, and individuals may experience these stages in varying orders and intensities.
The Psychological and Emotional Stages of Accepting Mortality
The process of accepting one’s mortality is rarely straightforward and often involves a complex interplay of emotions and psychological adjustments. Kübler-Ross’s five stages of grief – denial, anger, bargaining, depression, and acceptance – while initially developed for those grieving the loss of a loved one, are often relevant to individuals facing their own end-of-life. However, it’s crucial to remember that not everyone experiences all stages, nor do they necessarily progress through them in a linear fashion.
Individuals may fluctuate between stages, experience them simultaneously, or skip some entirely. For example, someone might initially experience denial, followed by periods of anger and bargaining interspersed with acceptance, before eventually finding a sense of peace. The intensity and duration of each stage also vary significantly depending on individual personality, spiritual beliefs, and the nature of the illness.
The Importance of Grief Counseling and Support Groups
Grief counseling and support groups provide invaluable resources for individuals facing end-of-life issues and their families. These services offer a safe and supportive environment where individuals can process their emotions, share their experiences, and learn coping mechanisms. Professional grief counselors can provide guidance and support in navigating the complex emotional landscape associated with death and dying. Support groups, composed of individuals sharing similar experiences, offer a sense of community and understanding, reducing feelings of isolation and allowing for mutual support.
The structured setting of a group, combined with the shared experience, can often lead to significant emotional relief and improved coping strategies. For example, a support group might provide a space for individuals to share their anxieties about the future, their concerns about their loved ones, or their fears about the dying process itself.
Common Emotional Responses of Family Members and Loved Ones, Final wishes and advance directives
Family members and loved ones often experience a profound range of emotions during the dying process of a loved one. These can include sadness, anger, guilt, fear, anxiety, and even relief. Sadness is a natural response to loss, while anger may stem from feelings of helplessness or resentment towards the illness. Guilt can arise from unresolved conflicts or perceived failures to provide adequate care.
Fear and anxiety often surround the uncertainty of the future and the practicalities of dealing with the death. In some cases, a sense of relief might be present, particularly if the loved one has experienced prolonged suffering. The intensity and manifestation of these emotions vary widely depending on the relationship with the dying person, individual coping mechanisms, and the circumstances surrounding the death.
For instance, a family member might experience intense guilt if they feel they haven’t spent enough time with their loved one in their final days.
Coping Mechanisms for Individuals and Families
Coping with the death of a loved one is a deeply personal process. Effective coping mechanisms often involve a combination of practical steps and emotional support. Practical steps might include arranging funeral arrangements, managing legal and financial matters, and seeking support from friends and family. Emotional coping strategies can include journaling, engaging in creative activities, practicing mindfulness, or seeking professional therapy.
Remembering positive memories and celebrating the life of the deceased can also be helpful. For example, creating a scrapbook of photos and memories can provide comfort and a tangible way to honor the deceased. Families might find solace in sharing stories and reminiscing about positive experiences with the deceased, helping to alleviate feelings of loss and isolation.
Resources Available for Individuals Dealing with Death and Dying
Several resources are available to support individuals and families dealing with death and dying.
- Hospice care: Provides comprehensive medical, emotional, and spiritual support for individuals in their final stages of life.
- Grief counseling: Offers professional guidance and support in navigating the emotional challenges of grief and loss.
- Support groups: Provide a supportive community for individuals sharing similar experiences.
- Online resources: Numerous websites and online communities offer information, support, and resources for those grieving.
- Religious organizations: Many religious organizations offer spiritual guidance and support to individuals and families during times of grief and loss.
Practical Considerations for End-of-Life Planning
Planning for the end of life can feel daunting, but proactively addressing practical considerations can significantly ease the burden on your loved ones and ensure your wishes are respected. This involves several key areas, including funeral arrangements, end-of-life care choices, financial planning, and decisions regarding burial or cremation. Careful consideration of these aspects allows for a more peaceful and organized transition.
Pre-planning Funeral Arrangements
Pre-planning funeral arrangements offers significant benefits. It allows individuals to personalize their services, reflecting their values and beliefs, while simultaneously relieving their families of difficult decisions during an already emotionally challenging time. Pre-planning often involves selecting a funeral home, choosing a casket or urn, deciding on the type of service (religious, secular, etc.), and specifying any desired music, readings, or other elements.
Many funeral homes offer pre-need arrangements, allowing individuals to pre-pay for services or set up payment plans to cover future costs. This eliminates financial stress for the family and ensures the chosen arrangements are executed according to the individual’s wishes.
Options for End-of-Life Care
Several options exist for end-of-life care, each designed to address different needs and preferences. Hospice care provides compassionate care for individuals with a life expectancy of six months or less. It focuses on pain management, symptom relief, and emotional support for both the patient and their family. Palliative care, on the other hand, can be provided at any stage of a serious illness, aiming to improve the quality of life by addressing physical, emotional, and spiritual needs.
It can be provided in various settings, including hospitals, nursing homes, and even at home. Choosing between hospice and palliative care depends on the individual’s prognosis and preferences.
Financial Planning for End-of-Life Expenses
Financial planning for end-of-life expenses is crucial. Costs can vary significantly depending on the chosen arrangements and location. These expenses include funeral and burial or cremation costs, medical bills, outstanding debts, and potential legal fees. Strategies for financial planning include creating a detailed budget, establishing a dedicated savings account, purchasing life insurance, or exploring options such as pre-paid funeral plans.
Openly discussing financial matters with family members ensures everyone is aware of the plans and can assist in managing expenses after the individual’s passing. It’s also advisable to keep all relevant financial documents organized and easily accessible for loved ones.
Burial and Cremation Options
Burial and cremation represent the two primary options for final disposition. Burial typically involves a traditional funeral service followed by interment in a cemetery plot. Various casket options exist, ranging in price and material. Cemetery plots can be purchased in advance or at the time of need. Cremation involves the reduction of the body to ashes, which can then be kept in an urn, scattered in a designated location, or placed in a niche within a columbarium.
Direct cremation, a simpler and less expensive option, omits the traditional funeral service. The choice between burial and cremation is deeply personal and should reflect the individual’s preferences and beliefs.
Cost Comparison of End-of-Life Options
| Option | Funeral Home Services | Casket/Urn | Burial/Cremation | Total Estimated Cost (USD) |
|---|---|---|---|---|
| Traditional Burial | $5,000 – $10,000 | $2,000 – $10,000 | $2,000 – $5,000 (plot, opening/closing grave) | $9,000 – $25,000+ |
| Direct Cremation | $1,000 – $3,000 | $500 – $2,000 | $500 – $1,500 | $1,500 – $6,500 |
| Cremation with Service | $3,000 – $7,000 | $500 – $2,000 | $500 – $1,500 (urn, scattering, niche) | $3,500 – $10,500+ |
| Green Burial | $1,000 – $4,000 | $500 – $1,500 (simple shroud or biodegradable casket) | $1,000 – $3,000 (plot in green burial cemetery) | $2,500 – $8,500 |
Planning for the end of life, while challenging, allows for greater control and peace of mind. By thoughtfully considering your final wishes and creating appropriate advance directives, you can ensure your preferences are respected and alleviate potential burdens on your loved ones. Open communication and proactive planning are key to navigating this sensitive subject matter with grace and dignity.
Remember, seeking professional legal and medical advice is crucial to ensure your documents are legally sound and tailored to your specific circumstances. Preparing for the future is an act of love for both yourself and those you leave behind.
Questions Often Asked
What happens if I don’t have an advance directive?
Without an advance directive, decisions about your medical care will be made by your family or a court-appointed guardian, potentially leading to treatments you wouldn’t have chosen.
Can I change my advance directive after it’s created?
Yes, you can revoke or amend your advance directive at any time as long as you have the capacity to do so.
Who should I involve in creating my advance directive?
It’s beneficial to discuss your wishes with family, friends, and your healthcare provider to ensure your preferences are understood and documented accurately.
Where can I find legal assistance with creating advance directives?
Consult an estate planning attorney or seek guidance from legal aid organizations specializing in end-of-life planning.






